Considerations When Managing Short Bowel Syndrome
Managing SBS usually includes a combination of strategies.
If you or someone you care for has SBS, it is important to play an active role in understanding SBS and establishing goals for management.
SBS management is complex and is adjusted to a person’s individual needs. Primary aims include:
Your healthcare team may use a combination of approaches to achieve the primary objectives in SBS management:

Diet
Surgery
Tube feeding
Medications
Intravenous nutrition and/or hydration
Caregivers of children with SBS: Check out our pediatric page to learn about management goals for children
SBS in ChildrenMaintaining Essential Nutrition and Hydration
There is no single “SBS diet”
Depending on the portion and length of your remaining bowel, and how well it functions, your doctor may help create a diet that’s tailored to you. Remember that different parts of the gastrointestinal tract absorb specific nutrients, so your diet will depend on your particular surgery.
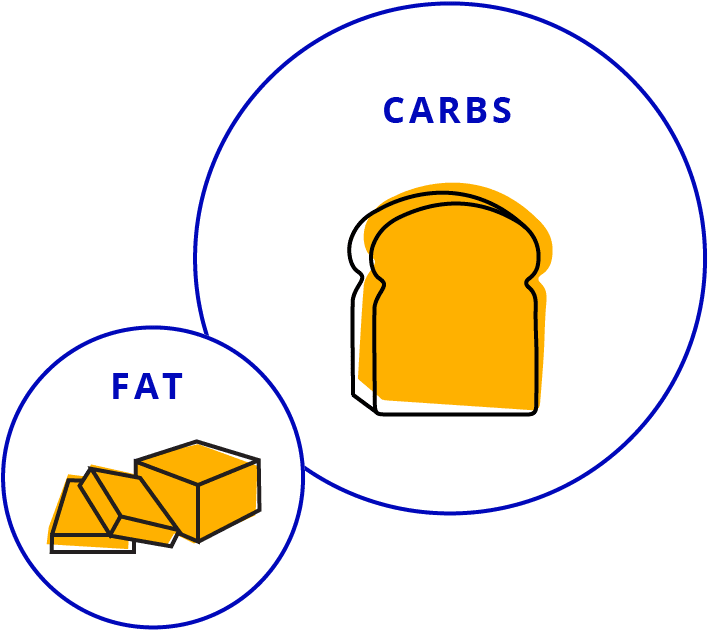
If you have any remaining colon
You may need to maintain a diet that is low in fat and high in carbohydrates.
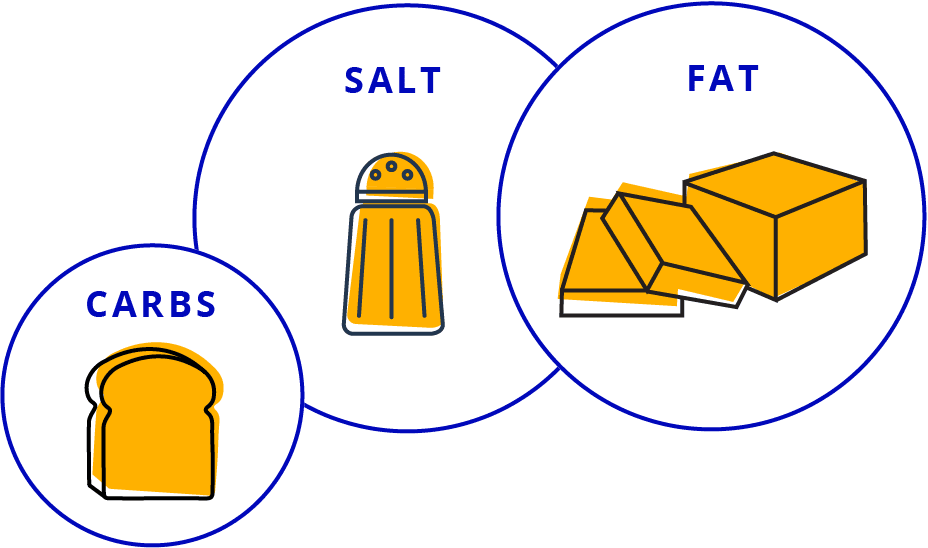
If you have a jejunostomy or an ileostomy
You may need to maintain a diet that is high in fat, low in carbohydrates, and higher in salt.
Remember to always talk to your doctor before changing your diet.
Learn more about the digestive system and how it processes food
Download PDF
For more on SBS and diet, sign up to receive a free guide by Carol Rees Parrish, MS, RDN; a registered dietitian with over 30 years experience helping people manage SBS.
Sign up nowStaying hydrated
Dehydration can be a serious concern. However, battling dehydration isn’t a matter of simply drinking more water. In fact, this can make the problem worse by increasing diarrhea or ostomy output. It’s important to consult your doctor when you notice signs of dehydration. This isn’t a problem that should be ignored!
Oral rehydration solution (ORS) is a simple, yet specific, solution of salt, sugar, and water that is used to aid in dehydration due to diarrhea. The special ratio of ingredients enhances absorption of fluid across the small bowel wall. Therefore, ORS will be absorbed even in the setting of diarrhea.
NOTE: This is not to be taken as medical advice. Ask your healthcare provider if these recipes or any ORS, are right for you and if volumes should be adjusted based on your specific fluid restrictions and needs.



SIP your way to hydration
When it comes to maintaining hydration remember to SIP–with advice from your HCP, follow a recipe to make an ORS from salt, sugars, and baking soda, include with water, then proactively drink slowly throughout the day. Drinking fast does not allow the intestine time to absorb the fluid, passing it out of the body too quickly. While there are many ORS products available to purchase, there are also recipes that can be made at home inexpensively.

For some ORS options to make at home, download this recipe book now.
Download pdf
“When I started understanding what I was living with, many things, like my struggles to stay hydrated for example, came into focus.”
Bethany, Living with SBS
GENERAL SBS EATING AND DRINKING TIPS
Unless otherwise instructed by your doctor, you should generally eat small and frequent meals to help manage certain SBS symptoms and encourage digestion and absorption. You’ll probably need to consume a lot more food and, ultimately, calories than someone with a normal-sized bowel would in order to compensate for your bowel’s inability to absorb nutrients normally.
- Track everything: write down what you eat and drink in a food diary
- Chew food thoroughly
- Eat smaller meals more often: eat up to 6 to 8 smaller meals each day, spaced out, eating the most nutritious foods first
- Limit fluids with meals: drink 4 ounces of fluid (about half a glass) or less at each meal, and stick with isotonic beverages like oral rehydration solutions

GENERAL FOODS TO AVOID
- Concentrated sweets: we know they’re tempting, but stay away from cookies, cakes, candies, chocolate, fruit drinks, honey, and syrups
- Alcohol and caffeine: these stimulate the GI tract
- High-oxalate foods (for people with a colon): like tea, instant coffee, cola drinks, nuts, soy products, leafy green vegetables, root vegetables, celery, berries, tangerines, rutabagas, and wheat germ (these can promote kidney stones)
- Osmotic carbohydrates: like fruit juice, colas, and simple sugars like cakes, cookies, pies, and donuts (these can pull water into the GI tract and lead to nutrition loss)
- Difficult-to-digest foods: like whole nuts, seeds, coconut, fruit skins/peels, and dried fruits

Remember to talk to your doctor before changing your diet.
For me, going out to eat is not going out to eat just because I like the food. It’s about going out to be with my friends and socialize.”

Improving Intestinal Adaptation
Helping the body compensate after surgery
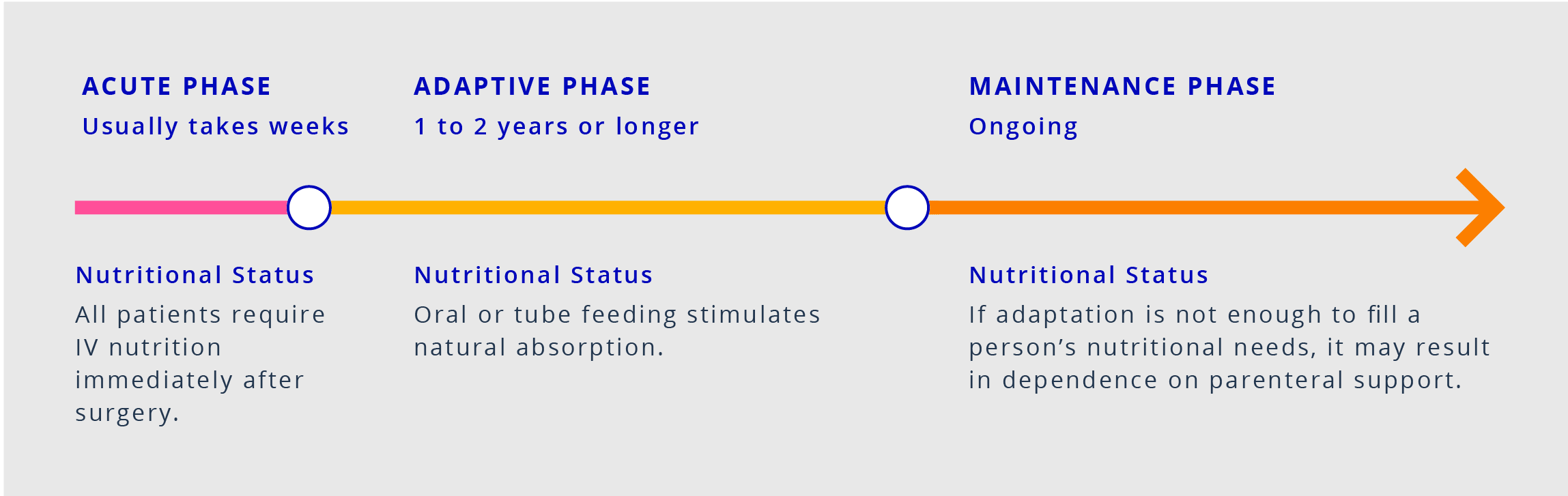
Intestinal adaptation begins naturally soon after surgery and may last 1 to 2 years, or sometimes longer. Adaptation involves changes to the structure and function of the remaining bowel, such as growth of new cells, as the body tries to compensate for the loss of intestine from surgery. The purpose is to increase nutrient and fluid absorption from the remaining bowel.
When possible after surgery, enteral feeding—that is, through the gut—should be prioritized over intravenous (IV) nutrition. The goal of oral and tube feeding is to stimulate and maintain or improve the intestine’s ability to absorb nutrients. You can observe the effects of adaptation through weight gain and stability of fluids and electrolytes.
Restoring the body’s natural ability to absorb nutrients is a key factor in returning people with SBS to as normal a lifestyle as possible. In addition to oral diet and hydration or tube feeding, your healthcare team may employ other methods to maximize gut function:
Medications
SBS medications may address SBS symptoms or improve intestinal adaptation. Their functions include:
- Slowing food transit and reducing diarrhea
- Reducing gastric secretions
- Treating bacterial overgrowth
- Increasing bowel growth and absorption
Surgery
Ostomy closures restore continuity for the GI tract, for example by reconnecting the small intestine to the colon, and are generally recommended when possible. Other nontransplant surgeries are used to slow movement of food, expand the surface area for absorption, or lengthen the remaining bowel. These latter surgeries are not common, and they can be challenging to perform.
Intestinal transplant is a last resort and generally only used when the person with SBS is suffering from life-threatening complications and is unable to continue on TPN.
No matter the approach, achieving intestinal adaptation—complete independence from parenteral support—is the goal in as many people with SBS as possible.
Reducing or Eliminating Parenteral Support (PS)
Weaning from PS can help avoid complications
Some people with short bowel syndrome (SBS) rely on PS for essential nutrition, and it is a lifesaving requirement following surgery. Some people with SBS experience life-threatening complications as a result of malabsorption and dependence on parenteral support.
This is a common PS complication. Signs and symptoms can include fever, feeling unwell, swelling and redness at the insertion site, increased sweating, chills, and pain in the insertion area.
Intestinal failure associated liver disease (IFALD) is a serious and potentially life-threatening complication that can occur in those on long-term parenteral nutrition. Small intestinal bacterial overgrowth and nutrient-specific factors such as lipid amount or composition are known to be drivers of IFALD development.
Use of PS over long periods of time can also affect the health and function of the kidneys, leading to difficulties in clearing the body of waste and toxins.
(high blood sugar)
Hyperglycemia is an increase in glucose (sugar) in the blood. It tends to occur more frequently when PS is being started and can be treated with insulin if necessary.
If the rate of fluid intake is too fast, or if all fluids haven’t been properly tracked, the result may be fluid overload. During the process of weaning off of PS, this is a potential risk as the bowel adapts and begins to absorb more. This complication can be prevented by properly monitoring all fluid intake.
PS can be lifesaving, but there are serious complications that can result from using it long term.
It is important to talk to your doctor about options to help you reduce or optimize your PS volume.
I worked with my doctor to wean off of TPN. It was a very gradual process and it took a lot of patience because you wanted to get to the end where you didn’t have any more.”

It’s not always possible for people who have had bowel resections to regain independence from parenteral support. Those who continue to depend on IV nutrition should talk to their doctors to find a routine that best supports their lifestyle.
Help minimize infections with careful hygiene, including:
- Washing your hands well
- Scrubbing the insertion point with alcohol for at least 15 seconds
- Stabilizing the line close to the site to avoid tugging
- Keeping the site clean and dry (promptly changing dressing after bathing or exercise)
Consider setting boundaries around handling your insertion site. Feel free to insist on handling your supplies yourself, even in a hospital.
Find more information on the Johns Hopkins Medicine and The Oley Foundation websites.*
Need to find a healthcare provider in your area with experience managing SBS?
Find a providerImproving Daily Life
The burden of SBS can be substantial, but there is hope
Living with SBS can sometimes feel like you’re tethered to the bathroom. Going from eating and drinking to tube feeding or TPN can be a difficult and uncomfortable adjustment for your body, resulting in a variety of possible complications.
Getting the hang of all your new medical equipment takes time. Dealing with clogged tubing or managing the pump can pose challenges. Learning how to sleep, use the bathroom, and have sex while hooked up to your equipment can also be trying.
While these adjustments can be difficult to manage, you are not alone. There are many others who are going through the same difficulties. It can be helpful to connect with these people through support groups and foundations.
No matter where I’ve lived, I’ve always had a garden. And having SBS is definitely not going to stop me from getting my hands in the dirt.”

The Oley Foundation is one place to find helpful resources and support*
Connect with others like you in our SBS Facebook community

Emergency Planning
A little bit of planning ahead of time can mean a world of difference in an emergency.
- If you have medical equipment that requires electricity, talk with your doctor or healthcare provider about how you can be prepared to use it during a power outage.
- If available, register with your local emergency management agency or office and understand any assistance that may be available. Registering is not a substitute for taking your own preparedness steps.
- Prepare with at least 1 week of prescription medicines.
- Have a copy of your prescriptions and information about dosing and administration.
- Prepare for any potential disruption in at-home medical services by speaking with your service provider about their emergency plans.
- Consider wearing a medical alert tag or bracelet.
For more information on planning for an emergency, visit Ready.gov.
*The links are provided as a resource. This is not an endorsement and Takeda has no control over the content of any website not owned by Takeda.
Building a support circle can help ensure that you meet your goals for living with SBS.